iTIND Therapy
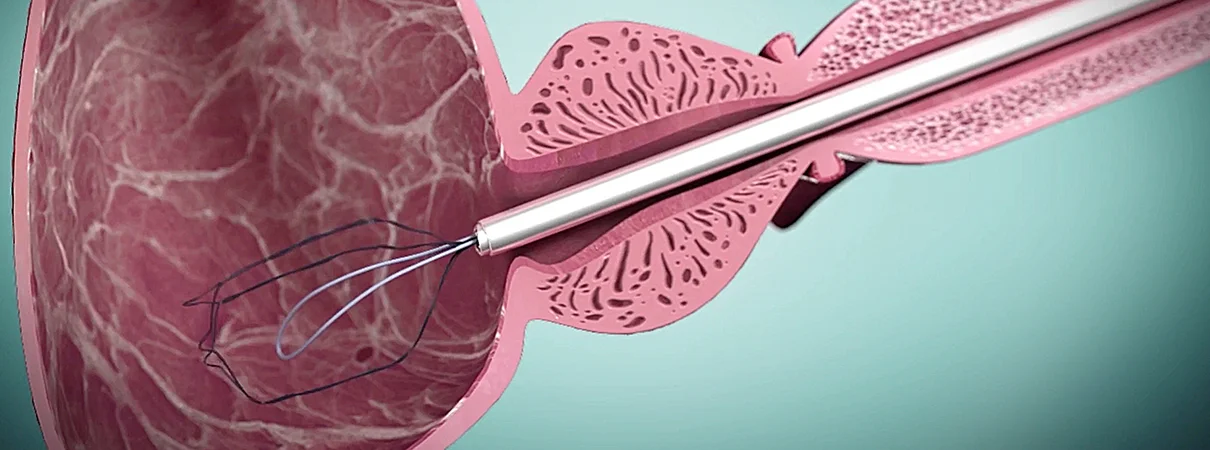
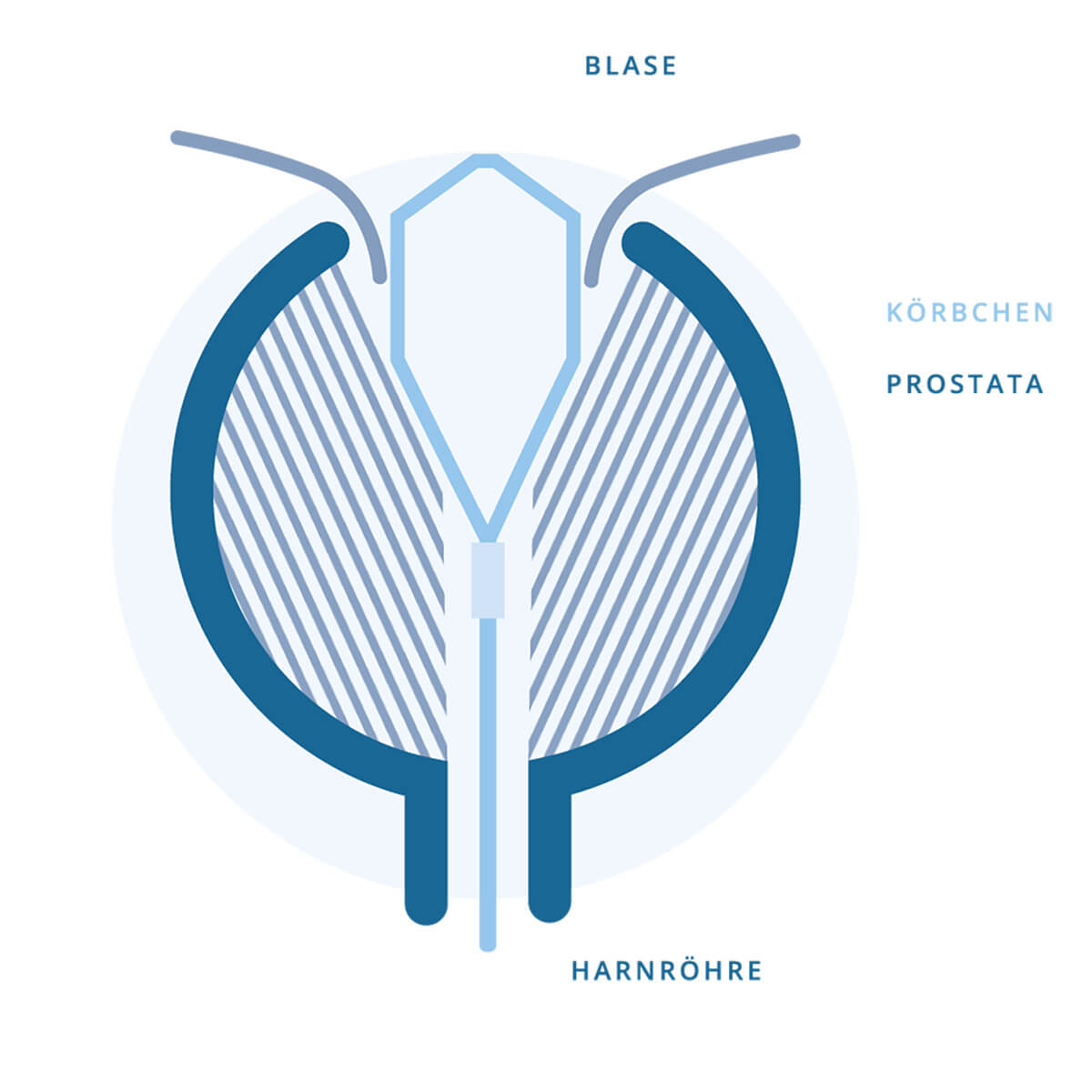
A small basket widens the prostate
Benign prostatic enlargement is a common condition in older men and affects over 30 million men in Europe and the USA in the context of lower urinary tract symptoms (LUTS) [1]. As a result of impaired bladder emptying, recurrent urinary tract infections and damage to the bladder and kidneys may occur over time. Initial treatment involves medication. In about 25% of patients this conservative therapy does not sufficiently relieve symptoms or has to be discontinued due to side effects [1,2]. In such cases, a range of surgical and interventional options is available.
Transurethral resection or laser enucleation of the prostate currently represent the subsequent standard of care. However, these operations are associated with non-negligible side effects. Typical complications include prolonged hospital stay, transfusions (2–8.4%), persistent incontinence (1.5%), and ejaculatory disorders (85%) [3,4].
An alternative method is iTIND (temporarily implantable nitinol basket), a basket that is temporarily placed in the prostate to widen the narrowing within the gland.
Questions and answers about the iTIND therapy (FAQ)
HOW DOES iTIND WORK?
iTIND is a basket that is inserted into the prostatic fossa via the urethra during cystoscopy (bladder endoscopy). The basket remains in place for 5 to 7 days and presses into the tissue during this time. Due to ischemia and necrosis, three longitudinal channels are formed and the bladder neck is widened. While the basket is in place, a small retrieval thread exits the urethra and is secured to the penis. After 5 to 7 days, the basket is collapsed in the prostate and removed via a catheter using the thread.
WHAT COMPLICATIONS CAN OCCUR?
There is no risk of injury to the ejaculatory ducts or the urinary sphincter. Therefore, there is no risk of incontinence or sexual dysfunction. In addition, compared with classic surgical methods such as TUR of the prostate, iTIND prevents the risk of retrograde ejaculation (absence of normal ejaculation) or incontinence [5]. During the time the basket is in place, mild bleeding, urinary frequency/urgency, and a pressure sensation in the perineal area are common. Urinary retention or infection can occur rarely. Overall, all symptoms are described as mild.
WHAT ARE THE RESULTS AFTER iTIND THERAPY?
Symptoms, measured by the IPSS (International Prostate Symptom Score), improve by an average of 13.7 points, and urinary flow measured by uroflowmetry improves by 7.4 ml/s [5]. These results were confirmed at 3-year follow-up.
WHO IS iTIND SUITABLE FOR?
iTIND is suitable for patients who:
- wish to preserve their sexual function
- are seeking an alternative medical therapy for BPH or for whom medication is insufficient
- are seeking an alternative to conventional surgery or are not suitable candidates for conventional surgery
- want to return quickly to everyday life after the procedure
- are looking for a low-complication treatment for benign prostatic hyperplasia
- have mild to moderate symptoms
- have a prostate size up to 70 g
- have a median lobe smaller than 1 cm
How should I behave after surgery for a spermatocele?
After the operation, several days of relative bed rest with scrotal elevation and consistent cooling are recommended. Your doctor will check the wound and assess the testicle by ultrasound.
The basket remains in the prostate for a few days and thereby displaces excess tissue.
Video on iTINDwith a symbolic illustration of the procedure
References
1. Roehrborn CG. Current medical therapies for men with lower urinary tract symptoms and benign prostatic hyperplasia: achievements and limitations. Rev Urol. 2008.
2. Verhamme KMC, Dieleman JP, Bleumink GS, Bosch JLHR, Stricker BHC, Sturkenboom MCJM. Treatment Strategies, Patterns of Drug Use and Treatment Discontinuation in Men with LUTS Suggestive of Benign Prostatic Hyperplasia: The Triumph Project. Eur Urol. 2003. doi:10.1016/S0302-2838(03)00376-2
3. Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol. 2011 Nov;186(5):1972-6.
4. Arbeitskreis Benignes Prostatasyndrom (AK BPS) der Akademie der Deutschen Urologen, S2e Leitlinie: Therapie des Benignen Prostatasyndroms (BPS) 2014; currently under revision
5. Porpiglia F, Fiori C, Bertolo R, et al. 3-Year follow-up of temporary implantable nitinol device implantation for the treatment of benign prostatic obstruction. BJU Int. 2018. doi:10.1111/bju.14141