Laser Enucleation of the Prostate (HoLEP/ThuLEP)
LOW-BLEEDING AND EFFECTIVE LASER THERAPY
In recent years, laser enucleation of the prostate has become the standard in many hospitals for the surgical treatment of benign prostatic enlargement. The procedure offers excellent effectiveness for any prostate size with a favorable risk profile compared with conventional methods such as transurethral resection of the prostate (TURP) or removal of the prostate via the lower abdomen (open surgery or robot-assisted with the da Vinci system).
Questions and answers on laser enucleation of the prostate (FAQ)
HOW DOES LASER ENUCLEATION WORK?
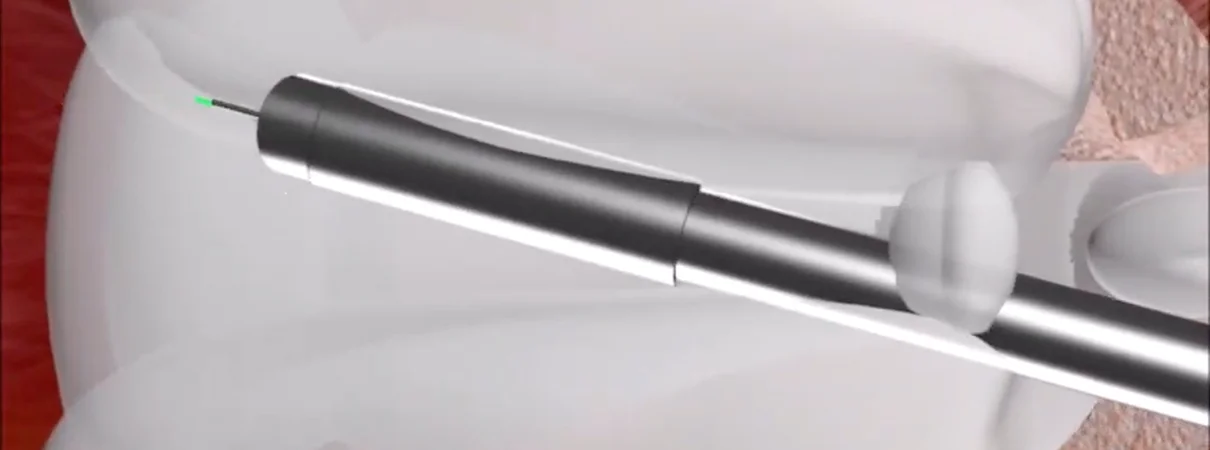
During laser enucleation, the instrument is first inserted through the urethra past the prostate into the bladder. The prostate is then incised with the laser, and the enlarged portion is separated from the capsule and the outer zone. The hollowed-out prostate tissue is brought into the bladder and there fragmented and suctioned using a special instrument (morcellator). All tissue is subsequently examined by a pathologist. Finally, a bladder catheter is placed to allow bladder irrigation so that no blood clots form after the surgery.
HOW LONG IS THE HOSPITAL STAY?
The patient is admitted on the day of surgery. The duration of the procedure depends on prostate size and is often under one hour. As a rule, discharge takes place after two nights in hospital. A further overnight stay is very rarely necessary. In individual cases, discharge may be possible after just one night.
WHAT HAPPENS DURING THE INPATIENT STAY?
After the operation, the patient is monitored for one to two hours in the recovery room. Afterwards, they return to the ward—eating and drinking is usually not a problem. However, physical activity should be avoided on the day of surgery, as a catheter remains in the urethra and the bladder is irrigated with water until the next morning. Patients often have mild difficulty with bowel movements; to help with this, stool softeners are routinely provided. Postoperative pain is very rare and easily treated. On the second day after surgery, the urethral catheter is removed—patients can urinate independently again and are discharged after a final check-up.
WHAT SHOULD BE CONSIDERED AFTER THE LASER PROCEDURE?
For four to six weeks:
- avoid strenuous exercise and cycling
- avoid thermal baths and saunas
- prevent constipation by adjusting your diet
- do not lift more than five kilos
- no sexual intercourse for the first two to three weeks
A temporary urge to urinate is common after laser treatment of the prostate. Even though the operation usually proceeds without problems, the enucleated prostate leaves a wound cavity through which urine flows. This causes irritation that can persist for several weeks. Depending on the severity of the benign prostatic syndrome, stress incontinence may occur due to an imbalance between the bladder muscle and the sphincter. This can be improved with pelvic floor training.
WHAT ARE THE RESULTS AFTER HOLEP?
Symptoms measured by the IPSS (International Prostate Symptom Score) improve to 1.7–5.2 points. Maximum urinary flow improves to 21.8–27.9 ml/sec. This means laser treatment of the prostate offers excellent effectiveness. Compared with transurethral resection of the prostate (TURP), HoLEP is more effective, leads to fewer bleedings and transfusions, and does not cause TUR syndrome (electrolyte shifts in the blood), which can be life-threatening [1,2]. HoLEP also results in a shorter postoperative catheterization period and a shorter hospital stay than TURP. Long-term outcomes show low rates of bladder neck contractures (0.8%), urethral strictures (1.6%), and reoperation due to residual prostatic enlargement (0.7%) [3]. Serious complications, such as injury to the sphincter or morcellation of the bladder wall, are extremely rare. Comparative studies between HoLEP and ThuLEP have shown both laser techniques to be equivalent.
WHO IS HOLEP/THULEP SUITABLE FOR?
- Patients with moderate to severe symptoms
- Any prostate size
- High-risk patients on anticoagulant therapy
- Patients with recurrent urinary tract infections
- Patients with bladder stones
- Patients with impaired kidney function
- Patients with a bladder diverticulum
- Patients with chronic prostatitis
WHICH LASER IS USED FOR THE OPERATION, AND WHAT ARE THE ADVANTAGES?
Two different lasers are available for the procedure. A classic, pulsed 100-watt Sphinx holmium laser from LisaLaser. This holmium-crystal-based solid-state laser has the excellent property of displacing tissue, allowing the enlarged inner portion of the prostate to be separated well from the capsule. However, it has slight weaknesses in achieving rapid hemostasis. By contrast, a classic continuous thulium laser provides very good coagulation, but it does not displace tissue—it “cuts” it.
In 2019, these two properties were technically combined in a pulsed thulium laser. Therefore, all operations at our center are performed with the RevoLix HTL from LisaLaser.
IS THE ABILITY TO EJACULATE PRESERVED?
An important aspect when deciding on HoLEP surgery is the question of ejaculation preservation. With the classic surgical technique, a high proportion of cases result in the absence of antegrade ejaculation (retrograde ejaculation). Most studies report very high rates of this, often over 70–90%. This effect has no influence on libido or erectile function, but may be relevant for many patients.
In recent years, special techniques have been developed that specifically preserve the structures in the area of the seminal tubercle (colliculus seminalis). These procedures—often referred to as ejaculation-preserving HoLEP—can significantly improve ejaculation preservation. Depending on the technique and patient population, studies have reported preservation rates of between approximately 50% and over 80%. [4]
It is important to understand that:
In order to protect ejaculation, more prostate tissue must be deliberately left in certain areas. Depending on the individual findings, this can have a moderate impact on the maximum effectiveness or long-term sustainability of the procedure. In many cases, however, the functional relief of the bladder remains very good, making this technique particularly suitable for patients for whom the preservation of ejaculation is important.
The prostate is incised with the laser and the enlarged portion is separated from the capsule and the outer zone.
Video on the topicLaser enucleation of the prostate
References
1. Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, Speakman MJ, Stief CG. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010 Sep;58(3):384-97.
2. Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S. A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update. Eur Urol. 2015 Jun;67(6):1066-1096.
3. Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of follow-up. J Urol. 2011 Nov;186(5):1972-6.
4. Suh YS et al. Ejaculatory preservation technique during holmium laser enucleation of the prostate: Functional and perioperative outcomes. World J Urol. 2021;39:1793